Cavitational Surgery
Cavitations (also called NICO lesions) are hollow places in the bone where a tooth used to be. These hollow areas may never cause pain or a problem. However, cavitations can produce trigeminal pain, headaches, and facial pain. Cavitations can also be found in other areas of the body, in any bones that contain marrow. Many oral cavitations linger for years without producing facial pain.
Most people know what we mean when we say cavity, but the word cavitation is confusing. Both of these words come from the same root word meaning hole. A cavity is a hole in the tooth, whereas a cavitation is a hole in bone. Unlike most tooth cavities, bone cavitations can’t be detected by simply looking at the bone, and even using x-rays, many cavitations are missed.
The termed cavitation was coined in 1930 by an orthopedic researcher to describe a disease process in which a lack of blood flow into the area produced a hole in the jawbone and other bones in the body.
Dr. G.V. Black, the father of modern dentistry, described this cavitation process as early as 1915 where he described a progressive disease process in the jawbone, which killed bone cells and produced a large cavitation area or areas within the jawbones.

He was intrigued by the unique ability of this disease to produce extensive jawbone destruction without causing redness in the gingiva (gums), jaw swelling, or an elevation in the patient’s body temperature. Essentially, this disease process, which produces osteonecrosis (dead bone) is actually a progressive impairment which produces small blockages (infarctions) of the tiny blood vessels in the jawbones, thus resulting in osteonecrosis, or areas of dead bone. These dead, cavitational areas, which produce pain, are now called NICO (Neuralgia Inducing Osteonecrosis) lesions. In his book on oral pathology, Dr. Black suggested surgical removal of these dead bone areas.
Dr. Jerry Bouquot, founder of has done a tremendous amount of recent scientific research on cavitations.
Chronic jaw pain
Cavitations may be the cause of chronic jaw pain.
Note: Some of the following material was written by Dr. Karen Shrimpken and others
A cavitation is a hole in the bone that cannot be detected through visual inspection and is poorly detected by x-rays. The term “cavitation” was coined to describe the result of a disease process in which the lack of blood supply to an area resulted in a hole or “hollowed out” portion of the jawbone or other bones in the body. Dr. G.V. Black described this process as early as 1915. He investigated how this disease produces extensive jawbone destruction without causing redness, swelling or increasing the patient’s body temperature.
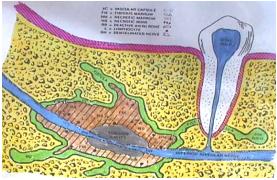
An illustration showing how a cavitation can eat away at the bone supporting teeth, and spread.
This disease progressively impairs the blood supply to the bone marrow in the jawbone resulting in osteonecrosis (bone death). The cause might be a biofilm form of bacteria that is antibiotic resistant and adheres to blood vessels. The released toxins & by-products from these bacteria, combined with cellular material, might be responsible for the lesions. Dr. Black recommended surgical removal of this dead, necrotic tissue to promote healing of the jawbone.
The term “cavitation” is generally used to describe lesions appearing as empty holes in the jawbone. They are usually ischemic (no oxygen supply), necrotic (dead), osteomyelitic (infected bone), and they usually release toxins. These lesions are often found in old extraction sites, under or near the roots of root canal teeth, avital (dead) teeth, and/or wisdom teeth. The lesion may spread throughout the jawbone, penetrate the sinuses or totally encompass the inferior alveolar (jaw) nerve.
Recent research by Dr. Boyd Haley, of the University of Kentucky, shows that ALL cavitation tissue samples tested contain toxins that significantly inhibit one or more of the enzymes used in the energy production cycle. These chemical toxins (most likely from anaerobic bacteria) can produce significant systemic effects, i.e. stopping the Krebs cycle at any one of a number of parts of the cycle. The Krebs cycle is responsible for energy production. This energy is what powers us in our day-to-day lives. Thus if you have no to poor energy production you may experience chronic fatigue.
Research has shown these toxins combine with chemicals or heavy metals, such as mercury, forming even more potent toxins. Research from German toxicologists indicates the jawbone may be a reservoir for chemicals and heavy metals (especially wisdom teeth sites). Clinically, it is easier to successfully detoxify the body of mercury after cavitations and mercury fillings are removed.
The term NICO (neuralgia-inducing cavitational osteonecrosis) has been used when severe facial pain, neuralgia, headache, or a phantom toothache accompanies this disease. Although the presence of cavitations is a common occurrence, only a small percentage of the individuals with cavitations suffer pain.
Even in the absence of pain or localized jawbone symptoms, systemic symptoms can be extensive. Researchers and physicians as early as 1918 expressed concern about the systemic effects of cavitations. A growing number of contemporary dentists, physicians, and researchers are even more alarmed by the latest research.
There are many possible initiating, predisposing, and risk factors associated with cavitations. A single or combination of factors can influence the occurrence, type, size, progression, growth pattern or symptoms resulting from a NICO lesion. Each individual is unique and each NICO lesion is uniquely located in a particular jawbone area making diagnosis and treatment complex. One of the major initiating factors is likely dental trauma, which includes physical, bacterial and toxic components.
Initiating Factors: Physical Trauma
As you will see, almost anything that can disrupt the bone tissue can act as an initiator.
- Extractions; dental injections; periodontal surgery; root canal procedures; grinding – bruxism; electrical trauma; metallic restorations; high speed drilling; bacterial trauma; periodontal disease; cysts; abscesses; root canal bacteria; dead teeth; improper cleaning after extractions; infected wisdom teeth or tooth buds (unerupted teeth)
- Initiating Factors – Toxic Trauma: dental materials; root canal toxins; anesthetic by-products; vasoconstrictors in anesthetics; chemical toxins; bacterial toxins; other toxins
Predisposing Factors
A number of factors predispose people to cavitational type lesions. Clotting disorders such as thrombophilia, hypofibrinolysis and others (which may be undiagnosed) may lead to oxygen-depleted areas of bone. Up to 11% of older individuals may have major or complete blockage of arteries to the jaws.
Radiation or chemotherapy for cancer; systemic disease such as rheumatoid arthritis, lymphoma or bone dysplasia, osteoporosis, lupus, sickle cell disease, homocystinemia, Gaucher’s disease, hyperlipidemia, hemodialysis, gout or antiphospholipid antibody syndrome. Inactivity (bedridden, paraplegic); deficiency of thyroid or growth hormone, occupational hazards such as variable atmospheric pressures can all be predisposing factors.
Risk factors
Many different factors put an individual at risk for ischemic osteonecrosis/NICO including corticosteroid use, pregnancy, estrogen use, alcoholism, cigarette smoking, and pancreatitis.
- For histological analysis
- For a sufferers viewpoint see this book, available in the office. Beyond Amalgam by Suzin Stockton.
Wisdom Teeth Extraction Sites
One source of data indicates that 45% of all jawbone cavitations are located in the third molar area where wisdom teeth have been previously extracted. These areas are particularly susceptible because they contain small terminal blood vessels (microvasculature) and osteonecrosis is a disease of such vessels. Injections for dental procedures are often given near these areas. When local anesthetic with vasoconstrictor (i.e. epinephrine) is used, the blood and thus oxygen supply to the bone in these areas is reduced. We recommend and use non-vasoconstricting anesthetics.
Prevention of Cavitations
Prevention involves the elimination or appropriate modification of initiating, predisposing, and risk factors. New technology, instruments, products and technological applications, may improve prevention and treatment and enhance the bone regeneration process. More research will improve the prevention, diagnosis and treatment of cavitations. Today, individuals can receive relief from local and systemic symptoms, diseases and pain by the surgical treatment of cavitations.
Recommended Treatment
Treatment of cavitations is to surgically scrape clean the area, removing all unhealthy bone and all diseased tissue such as abscesses, cysts, etc. After removing the unhealthy bone, the goal is bone regeneration. Successful bone regeneration relies on an individual’s healing capacity and the elimination and treatment of predisposing/risk factors. This is not always possible.
Failure to heal or reoccurrence of a lesion and the need for retreatment is always a possibility, no matter how well the surgery is performed. There are very few dentists who are trained to effectively diagnose and treat these lesions. Those who are not so trained are not qualified to diagnose this condition or confidently assure patients that they do not have cavitations.
Diagnosis of Cavitations
Diagnosis – the first step in successfully treating cavitations. Diagnosis can be made using a panoramic x-ray and kinesiology. One can view the upper jaw, lower jaw, teeth and sinuses on a large panorex x-ray. It does not always detect early stages of osteonecrosis in the bone, but many lesions can be seen on this type of x-ray.
Diagnostic Blocks
A relatively simple technique used to locate and confirm the presence of a NICO lesion. Here a few drops of non-vasoconstrictive anesthetic is injected into the gum tissue over a suspected site. Several minutes are allowed to pass and the pain pattern is evaluated for change. By doing this slowly and sequentially one can gain a greater awareness of the condition and location of the source lesion.
Preparation – Oral
Once the diagnosis is made and the need for surgical treatment determined the patients need to be prepared. Naturally, the oral cavity is the most germ-laden area of the body. Plaque, calculus, or periodontal disease only increases the severity of the problem. Prior to surgery the patient’s mouth, including the teeth, gums and tongue need to be as clean as possible. This may require a professional hygiene appointment at a dental office and diligent home care including brushing, flossing, rinsing, irrigating, and tongue scraping. Oral care products containing fluoride, alcohol, and sodium lauryl sulfate should be avoided.
Preparation – Systemic
There are several products, including enzymes, homeopathic lymphatic drainage remedies, natural antimicrobials, and healing nutrients that may provide nutritional and systemic support prior to and after the surgery. In some cases, limited antibiotics may be needed. It is important that all body detoxification pathways are open and functioning well; bowels, kidneys, skin, lungs, and especially the lymphatics. Electrolyte balance is important for detoxification and healing.
Surgical Procedure
A local anesthetic without vasoconstrictor is administered, because it is the least toxic and least damaging. Additionally, homeopathic antibiotics and pain interrupters are administered. An incision in the gum and bone is performed. Once access is gained then specimens are removed for biopsy testing.
At times it is necessary to remove an avital (dead) or root canal tooth. The instruments and procedures are used to help prevent contamination of the open bone area and to remove the necrotic (dead), osteomyelitic (infected) and toxic bone. This can be a slow and tedious process, especially when the necrotic bone surrounds the alveolar nerve or extends into the sinuses.
After the necrotic bone is removed, the surgical site is irrigated with various solutions to aid in the removal of bacteria and toxins. The area is closed with special sutures that help prevent bacterial growth.
Post Surgery
After surgery, intravenous vitamin C (IV-C) can assist with healing, cleaning up toxic materials and bacteria released into the bloodstream and detoxifying local anesthetics and IV medications. You can schedule this service with a holistic physician. Tenderness and soreness generally occur in the area of the surgery and can be controlled with pain medication. Some swelling and bruising may occur. The area may ache during the healing process.
We recommend liquid diet the first day and soft foods the first week. Salt water and/or antimicrobial rinses, and continued oral hygiene are important. Sutures are removed 5 to 7 days after the surgery. If any indication of infection (swelling, fever, increasing pain) occurs, contact us immediately. The number of areas treated during one surgery depends on the number of lesions to be treated and the individual.
Other adjunctive therapies post surgically are: t he use of low level infrared laser therapy (Anodyne) and hyperbaric oxygen. This is applied immediately post operatively and can be used for continued daily home care for the next month. The frequency of light (860nm) emitted by the diodes was specially picked for the healing effects on the tissues. Tremendous amounts of research have been carried out on this particular system, which is why we have chosen to use it.
Low-Level Laser Therapy
We use an Anodyne unit. Here we place the pads on the affected area. The science behind this technology is complex but in simple terms we have:
- Increased circulation to the area being energized
- Production of Nitric Oxide (NO). A very body friendly molecule. It is small molecule composed of single atoms of nitrogen and oxygen. It is a biological mediator that communicates physiologic and pathophysiologic messages. It is synthesized from the amino acid L-arginine by a family of enzymes. This reaction occurs within the vascular endothelium and is responsible for vascular tone that is essential for the regulation of blood pressure. Thus the benefits of Nitric Oxide (NO) are:
- Relaxes smooth muscle tissue.
- Increases vasodilation to increase circulation
- Causes lymphatic dilation
- Is necessary for the formulation of new capillaries and cell migration in a wound site.
- Increases collagen synthesis and proper collagen fibril alignment.
- Increases the viability of cutaneous flaps
- Reduces swelling
- Is anti-viral
- Is anti-inflammatory
- Is an anti-bacterial agent
- Is important for new bone growth
- Is the direct mediator of the analgesic effects of morphine.








